Introduction
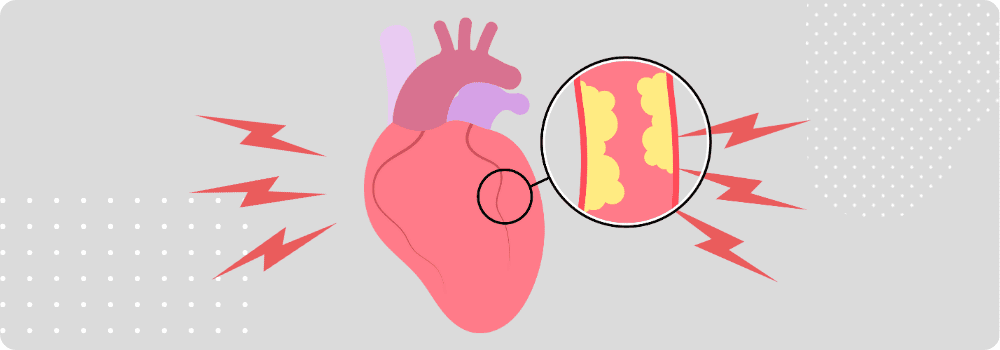
Angina, often described as chest discomfort or pressure, is a symptom of underlying heart disease rather than a disease itself. It occurs when the heart muscle does not receive enough oxygen-rich blood, usually due to narrowed coronary arteries. Recognizing angina is critical because it can signal coronary artery disease (CAD) or an increased risk of heart attack. This article delves into the different types of angina, their triggers, and effective treatment strategies, helping readers understand how to manage this condition and protect heart health.
What is Angina?
Angina is characterized by discomfort, pressure, or tightness in the chest that often radiates to the shoulders, arms, neck, jaw, or back. It typically arises when the heart’s demand for oxygen exceeds the supply, a condition medically known as myocardial ischemia. Angina can vary in intensity, duration, and frequency depending on the underlying cause and individual health factors.
Types of Angina
Angina is generally classified into four main types:
1. Stable Angina
- Definition: Predictable chest discomfort that occurs with exertion or emotional stress and usually subsides with rest or medication (like nitroglycerin).
- Symptoms: Pressure, heaviness, or tightness in the chest lasting 5–15 minutes.
- Triggers: Physical activity, stress, cold weather, heavy meals.
- Significance: Often indicates underlying coronary artery disease but is generally manageable with lifestyle changes and medication.
2. Unstable Angina
- Definition: Chest pain that is unpredictable, occurs at rest or with minimal exertion, and may worsen over time.
- Symptoms: Sudden, severe chest discomfort lasting longer than 15 minutes, often unrelieved by rest or usual medications.
- Significance: A medical emergency. Unstable angina can precede a heart attack and requires immediate medical attention.
3. Variant (Prinzmetal’s) Angina
- Definition: Rare type caused by a temporary spasm in the coronary arteries rather than a blockage.
- Symptoms: Chest pain typically occurs at rest, often at night or early morning, and may be intense.
- Triggers: Smoking, stress, exposure to cold, certain medications, or stimulant use.
- Significance: Can be treated effectively with medications that relax the coronary arteries.
4. Microvascular Angina
- Definition: Caused by abnormalities in the tiny blood vessels of the heart (microvasculature), more common in women.
- Symptoms: Chest pain or discomfort that may be severe and prolonged, often without major coronary artery blockages.
- Significance: Can be harder to diagnose and treat than other forms of angina but still responds to lifestyle modifications and certain medications.
Common Triggers of Angina
Angina occurs when the heart’s oxygen demand exceeds supply. Common triggers include:
- Physical exertion: Exercise, climbing stairs, or lifting heavy objects.
- Emotional stress: Anxiety, anger, or excitement can increase heart workload.
- Cold temperatures: Cold weather can constrict blood vessels.
- Heavy meals: Large meals redirect blood flow to the digestive system.
- Smoking and stimulants: Nicotine and caffeine can narrow arteries and increase heart rate.
- Medical conditions: Anemia, high blood pressure, or fever can exacerbate angina.
Understanding personal triggers is crucial for managing symptoms and preventing complications.
Symptoms of Angina
While chest discomfort is the hallmark, angina can manifest in various ways:
- Chest pressure, tightness, or squeezing
- Pain radiating to the arms, neck, jaw, back, or stomach
- Shortness of breath
- Fatigue
- Nausea or lightheadedness
- Cold sweats
It’s important to recognize that symptoms may differ between men and women; women often experience more subtle signs like unusual fatigue, indigestion, or jaw pain.
Diagnosis of Angina
Doctors diagnose angina based on:
- Medical history: Symptom patterns, triggers, and family history of heart disease.
- Physical examination: Checking blood pressure, heart rate, and other indicators.
- Electrocardiogram (ECG/EKG): Detects abnormal heart rhythms and signs of reduced blood flow.
- Stress tests: Exercise or medication-induced stress to evaluate heart function.
- Imaging tests: Echocardiogram, coronary angiography, or CT scans to visualize arteries.
- Blood tests: Assess cardiac enzymes if a heart attack is suspected.
Accurate diagnosis is essential to differentiate angina from other conditions like acid reflux or musculoskeletal pain.
Treatment of Angina
Treatment strategies aim to reduce symptoms, improve quality of life, and prevent heart attacks.
1. Lifestyle Modifications
- Adopt a heart-healthy diet (low in saturated fats, rich in fruits, vegetables, and whole grains).
- Exercise regularly under medical guidance.
- Quit smoking and limit alcohol consumption.
- Manage stress through relaxation techniques, yoga, or therapy.
- Maintain a healthy weight and monitor blood pressure, cholesterol, and blood sugar.
2. Medications
- Nitrates (e.g., nitroglycerin): Relieve chest pain by dilating blood vessels.
- Beta-blockers: Reduce heart rate and workload.
- Calcium channel blockers: Relax arteries and reduce heart workload.
- Antiplatelet agents (e.g., aspirin): Prevent blood clots.
- Statins: Lower cholesterol to reduce plaque buildup.
- Ranolazine: Helps control chronic angina symptoms in certain cases.
3. Medical Procedures
For severe or unstable angina, interventions may be necessary:
- Angioplasty and stenting: Opens narrowed arteries to restore blood flow.
- Coronary artery bypass grafting (CABG): Reroutes blood around blocked arteries.
When to Seek Immediate Medical Attention
Seek urgent medical care if angina:
- Occurs at rest or with minimal exertion
- Becomes more frequent, severe, or prolonged
- Is accompanied by shortness of breath, nausea, sweating, or fainting
Unstable angina may indicate an impending heart attack, and every minute counts.
Conclusion
Angina is a warning signal that the heart is not receiving enough oxygen. Recognizing its types—stable, unstable, variant, and microvascular—along with understanding triggers and symptoms, allows for timely intervention. Effective management combines lifestyle modifications, medications, and, in some cases, medical procedures. By staying vigilant and proactive, individuals with angina can significantly reduce their risk of heart attacks and maintain a healthier, more active life.
FAQs:
What is angina?
Angina is chest discomfort or pain that occurs when the heart muscle doesn’t get enough oxygen-rich blood, often due to narrowed arteries.
What are the different types of angina?
The main types of angina are stable angina, unstable angina, variant angina (Prinzmetal’s), and microvascular angina.
What triggers angina?
Common triggers include physical exertion, stress, cold weather, large meals, smoking, and certain medications or stimulants.
How is angina treated?
Treatment often involves lifestyle changes, medications (e.g., nitrates, beta-blockers), and in severe cases, procedures like angioplasty or bypass surgery.
When should I seek medical help for angina?
Seek medical attention immediately if chest pain occurs at rest, lasts longer than usual, or is accompanied by shortness of breath, nausea, or sweating.