Introduction
Urge incontinence, also known as overactive bladder, is characterized by a sudden, intense urge to urinate, often leading to involuntary leakage. It can interfere with daily activities, sleep, and overall quality of life. While medications and lifestyle changes can help, bladder training is a first-line, non-invasive therapy proven to improve bladder control by teaching the bladder and brain to communicate more effectively.
This article provides a step-by-step guide to bladder training techniques for managing urge incontinence.
How Bladder Training Works
Bladder training involves gradually increasing the time between bathroom visits, teaching the bladder to hold urine for longer periods and reducing urgency episodes. The goal is to retrain the bladder, reduce overactivity, and restore confidence in managing urinary habits.
Step 1: Keep a Bladder Diary
Before starting, track your urinary habits for 3–7 days:
- Time of urination
- Amount of urine (optional, using a measuring container)
- Episodes of urgency or leakage
- Fluid intake
- Triggering activities
This diary helps identify patterns and sets a baseline for training.
Step 2: Establish a Timed Voiding Schedule
- Start with fixed intervals, such as every 60 minutes, even if you don’t feel a strong urge.
- Gradually increase the interval by 15–30 minutes each week, aiming for 2–4 hours between voids.
- Stick to the schedule consistently to condition the bladder to hold urine longer.
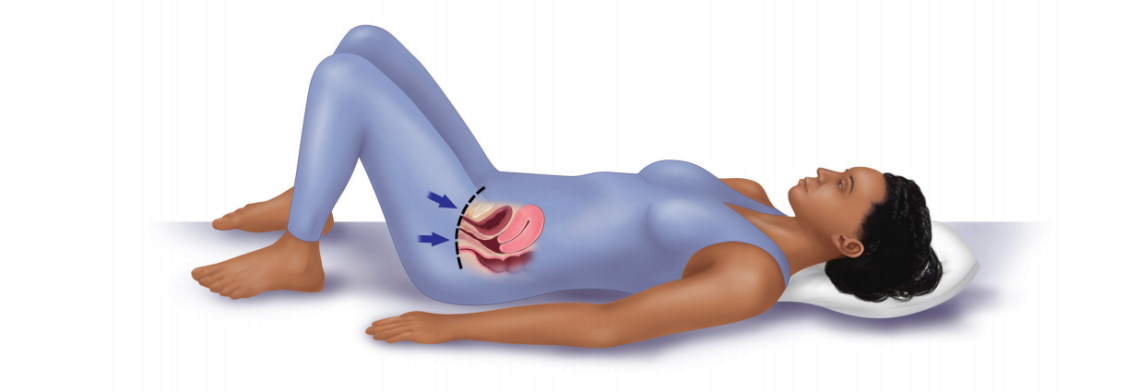
Step 3: Practice Urge Suppression Techniques
When you feel a sudden urge:
- Pause and contract the pelvic floor muscles (Kegels) to inhibit the urge.
- Distract your mind by counting, taking deep breaths, or walking slowly.
- Sit down or stand still, focusing on relaxation rather than rushing to the toilet.
Over time, these techniques help reduce urgency intensity.
Step 4: Modify Fluid and Diet Habits
- Avoid bladder irritants, such as caffeine, alcohol, artificial sweeteners, and carbonated drinks.
- Stay hydrated, but sip fluids throughout the day instead of drinking large amounts at once.
- Empty your bladder before sleep to reduce nighttime urgency.
Step 5: Combine with Pelvic Floor Exercises
- Strengthening the pelvic floor muscles enhances bladder control.
- Perform Kegel exercises regularly, especially before and during episodes of urgency, to suppress leaks.
Step 6: Monitor Progress
- Track intervals, urgency episodes, and leakage in your bladder diary.
- Gradually increase voiding intervals as the bladder adapts.
- Celebrate small improvements to stay motivated.
Tips for Success
- Be patient: Bladder training can take 6–12 weeks to show significant improvement.
- Stay consistent: Regular practice is essential for retraining the bladder.
- Seek professional guidance: A urologist, continence nurse, or pelvic floor physical therapist can provide individualized strategies.
- Combine therapies: Lifestyle modifications, bladder training, and pelvic floor exercises often yield the best results.
Conclusion
Bladder training is an effective, non-invasive method for managing urge incontinence. By establishing a structured voiding schedule, practicing urge suppression techniques, strengthening the pelvic floor, and adjusting lifestyle habits, individuals can regain bladder control and improve quality of life. While it requires patience and consistency, the long-term benefits of bladder training are substantial, reducing urgency episodes and helping people live confidently.
FAQs
1. How long does bladder training take to work?
Most people notice improvement within 6–12 weeks of consistent practice.
2. Can I drink fluids while doing bladder training?
Yes, staying hydrated is important, but sip water steadily rather than drinking large amounts at once.
3. What if I leak during bladder training?
Accidental leakage is common at first. Don’t get discouraged—consistency over time strengthens the bladder.
4. Can men and women both benefit from bladder training?
Yes. Bladder training is effective for both genders with urge incontinence.
5. Do I need professional help to start bladder training?
While you can begin on your own, guidance from a healthcare professional ensures proper technique, interval adjustments, and incorporation of pelvic floor exercises.