Introduction
Many people notice that abdominal pain and digestive discomfort often worsen during stressful times. This is not just a coincidence—the gut and the brain are deeply interconnected through what scientists call the gut-brain axis. Stress can directly influence how the digestive system functions, while gut issues can also affect mood and mental health. Understanding this two-way relationship helps explain why conditions like irritable bowel syndrome (IBS) are often linked with stress and anxiety, and why managing emotional health can play a vital role in reducing abdominal pain.
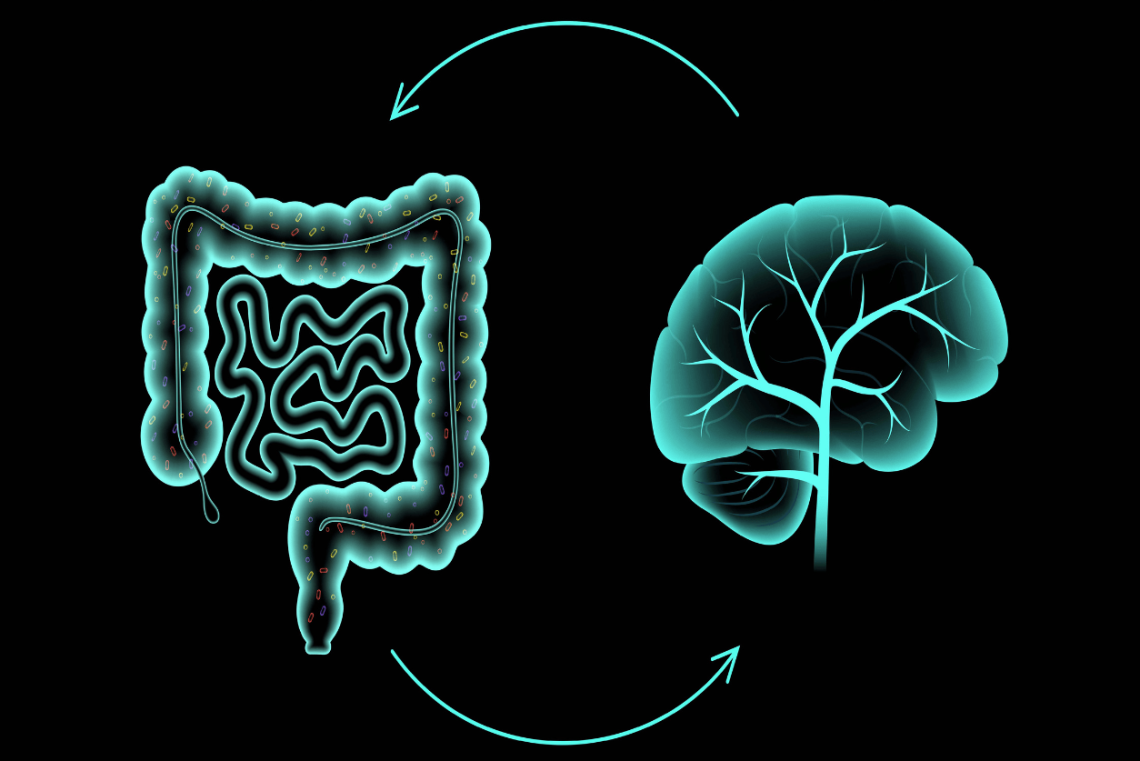
What Is the Gut-Brain Axis?
The gut-brain axis is the communication network that links the brain, the central nervous system, and the digestive tract. It works through:
- Nervous system connections: The vagus nerve carries signals between the brain and gut.
- Hormonal signals: Stress hormones like cortisol can alter gut function.
- Immune pathways: Inflammation in the gut can influence mood and brain activity.
- Gut microbiome: Trillions of gut bacteria produce neurotransmitters (like serotonin) that affect both digestion and mental health.
How Stress Affects the Gut
1. Changes in Digestion
Stress can speed up digestion, leading to diarrhea, or slow it down, causing constipation. This imbalance contributes to abdominal pain and discomfort.
2. Increased Sensitivity to Pain
Stress heightens nerve sensitivity in the gut, making normal sensations feel painful—a hallmark feature in IBS.
3. Altered Gut Microbiome
Chronic stress can disrupt the balance of gut bacteria, leading to bloating, cramping, and inflammation.
4. Reduced Blood Flow and Motility
Stress diverts blood flow away from the digestive organs, impairing normal digestion and nutrient absorption.
5. Muscle Tension
Stress causes abdominal muscle tightening, which can increase cramping and discomfort.
Conditions Linked to Stress-Related Abdominal Pain
Irritable Bowel Syndrome (IBS)
One of the most studied conditions in the gut-brain connection. Stress often triggers flare-ups of abdominal pain, bloating, and bowel habit changes.
Functional Abdominal Pain Disorders
Children and adults may develop chronic abdominal pain without visible disease, often linked to stress and gut sensitivity.
Gastroesophageal Reflux Disease (GERD)
Stress does not directly cause GERD, but it can worsen symptoms such as heartburn and abdominal discomfort.
Managing Stress to Reduce Abdominal Pain
1. Relaxation and Breathing Techniques
Deep breathing, meditation, and progressive muscle relaxation calm the nervous system and reduce gut sensitivity.
2. Cognitive Behavioral Therapy (CBT)
Helps people reframe negative thoughts and reduce stress-related gut symptoms.
3. Physical Activity
Regular exercise lowers stress hormones and improves bowel motility.
4. Dietary Adjustments
Avoiding trigger foods and following a low-FODMAP diet may help with IBS.
5. Adequate Sleep
Poor sleep worsens both stress and digestive symptoms—prioritize consistent rest.
6. Gut-Friendly Foods
Probiotics, prebiotics, and fiber-rich foods support gut health, which in turn improves resilience to stress.
When to See a Doctor
While stress is a common cause of abdominal pain, it is important to seek medical advice if you experience:
- Persistent or severe abdominal pain.
- Unexplained weight loss.
- Blood in stool or vomit.
- High fever with abdominal discomfort.
- Pain that wakes you from sleep.
These may indicate underlying medical conditions that require attention.
Conclusion
The connection between stress and abdominal pain is real and powerful, driven by the gut-brain axis. Stress can disrupt digestion, heighten pain sensitivity, and alter gut bacteria, leading to discomfort and chronic conditions like IBS. By addressing both mental and physical health—through relaxation techniques, dietary care, and lifestyle adjustments—people can often find significant relief. A healthy gut supports a healthier mind, and vice versa.
FAQs
1. Can stress alone cause abdominal pain?
Yes. Stress can increase gut sensitivity, alter motility, and trigger pain even without structural disease.
2. Why does IBS flare up during stressful times?
IBS symptoms worsen because stress affects the gut-brain axis, increasing nerve sensitivity and altering digestion.
3. Can relaxation techniques really help abdominal pain?
Yes. Breathing exercises, meditation, and yoga reduce stress signals that impact the gut.
4. Does the gut microbiome affect stress levels, too?
Yes. Gut bacteria produce neurotransmitters like serotonin, which influence both mood and gut function.
5. Should I see a doctor if stress-related pain doesn’t go away?
Absolutely. Persistent abdominal pain needs evaluation to rule out medical causes beyond stress.