Introduction
Topical hydrocortisone and other corticosteroid creams are widely used to treat inflammatory skin conditions such as eczema, psoriasis, and allergic reactions. Their anti-inflammatory and immunosuppressive properties provide quick relief from itching, redness, and swelling. However, despite being available over the counter and considered relatively safe when used appropriately, misuse and overuse of topical steroids can lead to serious health complications. One of the most insidious risks is systemic absorption leading to adrenal suppression, a potentially dangerous condition that affects hormone balance.
Additionally, abrupt discontinuation of prolonged topical steroid use can trigger withdrawal syndromes characterized by worsening skin symptoms. This article will explore how systemic absorption occurs, the mechanisms and symptoms of adrenal suppression, the phenomenon of topical steroid withdrawal, skin complications such as atrophy and rebound dermatitis, and finally, guidelines for safe use and alternatives for managing skin conditions.
Systemic Absorption of Topical Steroids
Although applied locally, topical steroids like hydrocortisone can be absorbed into the bloodstream, especially when used over large body areas, under occlusive dressings, on damaged or thin skin (such as the face or intertriginous areas), or for prolonged periods.
Factors increasing absorption include:
- High potency steroids
- Frequency and duration of application
- Skin barrier integrity
- Use on children or elderly with thinner skin
Systemic absorption can suppress the hypothalamic-pituitary-adrenal (HPA) axis, interfering with the body’s natural cortisol production.
Adrenal Suppression Mechanisms and Symptoms
Adrenal suppression occurs when exogenous corticosteroids reduce the body’s need to produce cortisol, a vital hormone for stress response, metabolism, and immune function.
Mechanisms
- Topical steroids absorbed into the bloodstream mimic cortisol effects.
- The pituitary gland senses excess corticosteroid, reducing adrenocorticotropic hormone (ACTH) secretion.
- Lower ACTH leads to decreased adrenal gland cortisol production.
- Prolonged suppression can cause adrenal atrophy and insufficiency.
Symptoms
- Fatigue and weakness
- Low blood pressure or dizziness
- Nausea and vomiting
- Muscle and joint pain
- Mood changes or irritability
- Severe cases risk adrenal crisis, a life-threatening emergency
Topical Steroid Withdrawal Syndrome
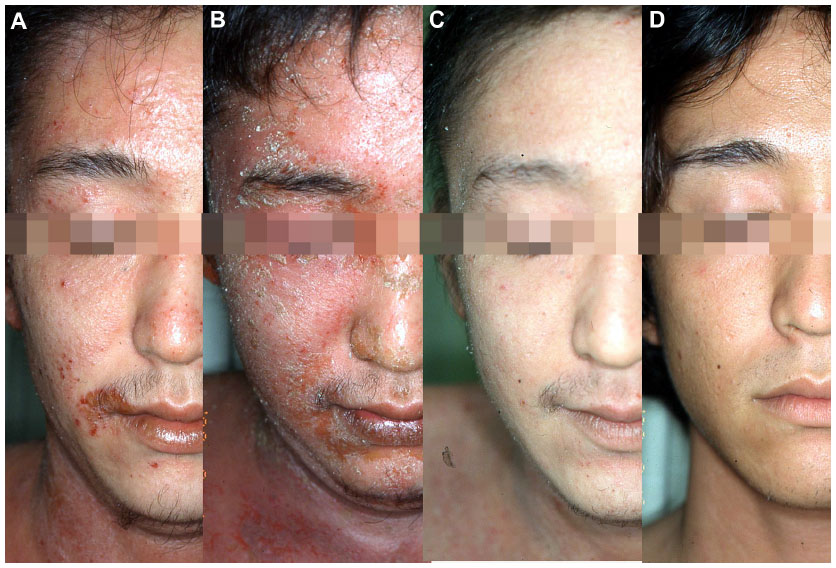
When long-term topical steroid use is stopped abruptly, some patients experience topical steroid withdrawal syndrome (TSWS), also known as red skin syndrome or steroid addiction dermatitis.
Symptoms
- Burning, stinging, or intense itching
- Redness and rash worsening beyond baseline
- Scaling, oozing, or swelling
- Flare-ups of original skin condition, sometimes more severe
TSWS may last weeks to months, significantly affecting quality of life.
Skin Atrophy and Rebound Dermatitis
Chronic topical steroid overuse also damages the skin directly:
- Skin Atrophy: Thinning of the skin, making it fragile, more prone to bruising, tearing, and delayed wound healing.
- Rebound Dermatitis: Skin inflammation that worsens after stopping steroids, often accompanied by severe itching and redness.
These complications may be irreversible if steroid use continues unchecked.
Safe Usage Guidelines and Alternatives
Safe Use Guidelines
- Use the lowest effective potency for the shortest duration possible.
- Follow healthcare provider instructions carefully.
- Avoid prolonged daily use without breaks.
- Do not apply to large body areas or under occlusion without medical advice.
- Monitor for early signs of side effects, such as thinning skin or stretch marks.
Alternatives and Adjuncts
- Non-steroidal topical treatments: Calcineurin inhibitors (e.g., tacrolimus), moisturizers, and barrier repair creams.
- Lifestyle and trigger management: Identifying and avoiding irritants or allergens.
- Phototherapy and other medical therapies for chronic conditions.
- Gradual tapering under medical supervision to avoid withdrawal symptoms.
Conclusion
Topical hydrocortisone creams and other steroids offer valuable benefits for managing inflammatory skin conditions, but their overuse carries hidden risks. Systemic absorption can suppress adrenal function, leading to potentially serious hormonal imbalances, while sudden cessation after prolonged use can trigger painful withdrawal syndromes. Additionally, chronic use damages the skin’s integrity, causing atrophy and rebound inflammation.
Awareness of these risks, adherence to safe usage guidelines, and exploring alternative therapies are essential steps to prevent the steroid cream trap. With proper medical guidance and cautious use, patients can enjoy the benefits of topical steroids without compromising their long-term health.
FAQs:
Can over-the-counter hydrocortisone cream cause adrenal problems?
Yes, if used excessively or over large areas, even low-potency OTC hydrocortisone can cause adrenal suppression, especially in children or with long-term use.
What are the signs of topical steroid withdrawal?
Redness, burning, stinging, intense itching, peeling, swelling, and worsening of the original skin condition after stopping steroid use.
How long is it safe to use hydrocortisone cream continuously?
Generally, no more than 1–2 weeks at a time unless directed by a doctor. Long-term daily use should be avoided.
What happens if I suddenly stop using steroid cream after long-term use?
You may experience rebound flare-ups or topical steroid withdrawal, including painful and inflamed skin symptoms.
Are there effective natural alternatives to topical steroids for skin conditions?
Yes, options include aloe vera, colloidal oatmeal, calendula, coconut oil, and barrier-repair moisturizers—though effectiveness varies and should be discussed with a healthcare provider.