Introduction
Familial hypercholesterolemia (FH) is a genetic disorder characterized by extremely high levels of low-density lipoprotein cholesterol (LDL-C), commonly known as “bad cholesterol.” Unlike typical high cholesterol influenced by lifestyle, FH is inherited and can lead to early-onset cardiovascular disease if left untreated.
Understanding FH, its signs, diagnosis, and management is crucial because early intervention can significantly reduce the risk of heart attacks and improve quality of life.
This article provides a comprehensive overview of familial hypercholesterolemia, helping individuals and families recognize the condition and take proactive steps for management.
What Is Familial Hypercholesterolemia?
FH is an inherited disorder caused by mutations in genes responsible for clearing LDL cholesterol from the bloodstream. The most common gene involved is the LDL receptor gene (LDLR), but mutations in other genes like APOB and PCSK9 can also cause FH.
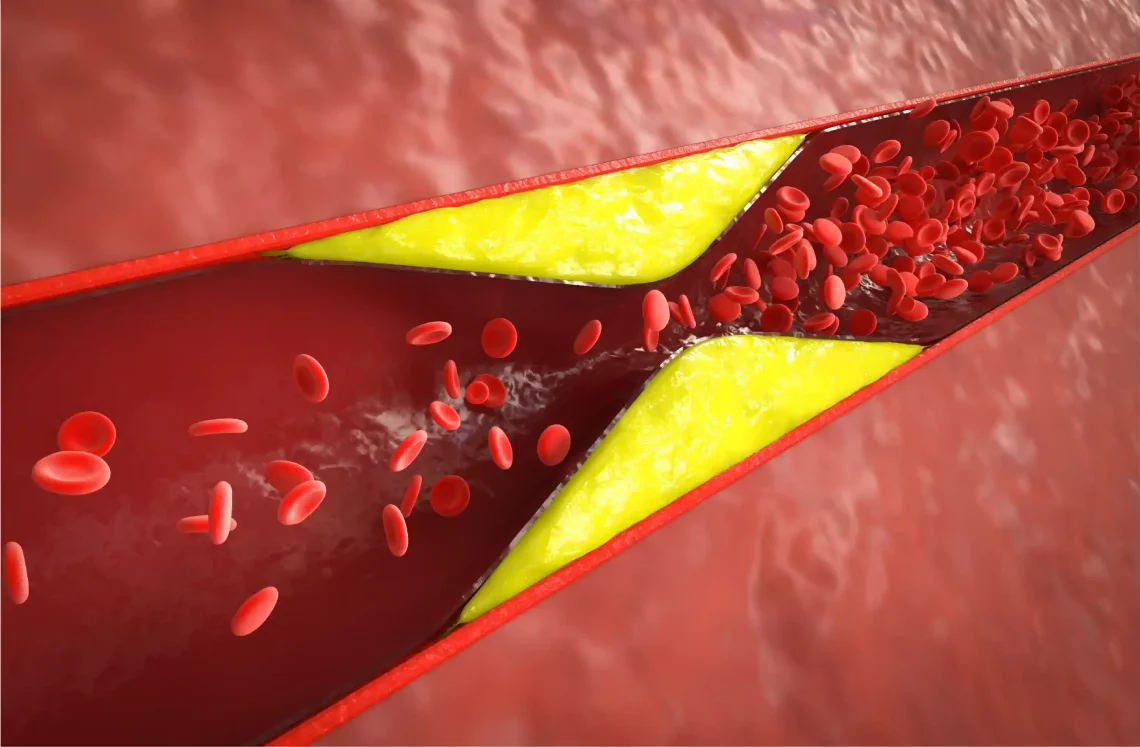
Because LDL receptors don’t function properly, LDL cholesterol builds up in the blood from birth, leading to:
- Extremely high LDL cholesterol levels (often >190 mg/dL in adults)
- Early development of atherosclerosis (artery plaque buildup)
- Increased risk of premature heart disease, often before age 55 in men and 65 in women
Types of Familial Hypercholesterolemia
1. Heterozygous FH (HeFH)
- Inherited from one parent.
- Affects about 1 in 250 people worldwide.
- LDL cholesterol levels typically range from 190 to 400 mg/dL.
- Heart disease risk is elevated but can often be managed with treatment.
2. Homozygous FH (HoFH)
- Inherited from both parents (very rare, about 1 in 300,000).
- LDL cholesterol levels can exceed 500 mg/dL.
- Severe cardiovascular disease often develops in childhood or adolescence.
- Requires aggressive treatment.
Signs and Symptoms
People with FH may not show symptoms until heart disease develops, but some physical signs include:
- Tendon xanthomas: cholesterol deposits in tendons (e.g., Achilles tendon, hands)
- Xanthelasmas: yellowish cholesterol deposits around the eyelids
- Corneal arcus: a white or gray ring around the cornea of the eye (especially in younger people)
Diagnosing Familial Hypercholesterolemia
Diagnosis involves a combination of:
- Family history of high cholesterol or premature cardiovascular disease
- Blood tests showing very high LDL cholesterol
- Physical examination for xanthomas and other signs
- Genetic testing to identify specific mutations (available but not always necessary)
Several clinical criteria exist, such as the Dutch Lipid Clinic Network Criteria, to help confirm diagnosis.
Why Early Diagnosis Matters
Early identification allows for timely intervention to:
- Lower LDL cholesterol levels effectively
- Prevent or delay heart attacks and strokes
- Screen and treat family members who may also have FH
Because FH runs in families, cascade screening (testing relatives) is recommended when someone is diagnosed.
Management and Treatment
Management of FH requires a lifelong, multi-faceted approach:
1. Lifestyle Modifications
- Heart-healthy diet low in saturated and trans fats, and rich in fruits, vegetables, and whole grains
- Regular physical activity
- Avoiding tobacco use
- Maintaining a healthy weight
While lifestyle alone usually isn’t enough, it supports medication effectiveness.
2. Medications
- Statins are the first-line therapy to reduce LDL cholesterol.
- Ezetimibe may be added if statins alone don’t reach LDL goals.
- PCSK9 inhibitors (e.g., evolocumab, alirocumab) are powerful injectable drugs for those with HeFH or HoFH not responding to standard treatment.
- Lomitapide and mipomersen are approved for HoFH in specialized settings.
- Bile acid sequestrants and other agents may also be used.
3. Lipid Apheresis
- For HoFH or severe HeFH, this procedure filters LDL cholesterol from the blood periodically.
- Typically used when medications aren’t sufficient.
Living with Familial Hypercholesterolemia
People with FH benefit from:
- Regular check-ups and lipid monitoring
- Early screening for cardiovascular disease (e.g., stress tests, imaging)
- Support from genetic counselors and specialists
- Awareness of symptoms indicating heart problems
Education and emotional support for patients and families are essential due to the lifelong nature of the condition.
The Importance of Family Screening
Because FH is inherited in an autosomal dominant pattern, each first-degree relative has a 50% chance of having the condition.
Cascade screening involves:
- Testing blood cholesterol levels of family members
- Genetic testing when available
- Early treatment to prevent complications
Current Research and Future Directions
New therapies targeting the genetic causes of FH and improving LDL clearance are under development, including:
- Gene therapy trials aiming to correct defective LDL receptor function
- Novel small interfering RNA (siRNA) therapies targeting PCSK9
- Advanced lipid-lowering agents with fewer side effects
These innovations hold promise for more effective, personalized FH management.
Conclusion
Familial hypercholesterolemia is a serious but manageable genetic disorder that significantly increases the risk of early cardiovascular disease. Early recognition through family history and testing, combined with aggressive cholesterol-lowering strategies, can help individuals with FH live longer, healthier lives.
If you have a family history of high cholesterol or premature heart disease, talk to your healthcare provider about screening for FH. Awareness and proactive management are key to reducing risks and protecting your heart.
FAQs:
What is familial hypercholesterolemia (FH)?
FH is an inherited genetic disorder causing very high LDL (“bad”) cholesterol levels from birth.
How is FH different from regular high cholesterol?
FH is caused by gene mutations and often leads to early heart disease, unlike cholesterol raised mainly by lifestyle.
What are the signs of FH?
Signs include very high cholesterol, tendon xanthomas (cholesterol deposits in tendons), and a family history of early heart disease.
How is FH treated?
Treatment includes lifestyle changes, statins, PCSK9 inhibitors, and sometimes advanced therapies like lipid apheresis.
Should family members be tested for FH?
Yes, because FH is inherited, relatives have a 50% chance of having the condition and should be screened early.