Introduction
Hemorrhoids, swollen veins in the anal and rectal region, affect millions of people globally. While many cases can be managed with lifestyle changes and home remedies, moderate to severe hemorrhoids often require medical intervention. Minimally invasive procedures have revolutionized hemorrhoid treatment, offering effective relief with less pain and quicker recovery than traditional surgery.
This article explores the most common minimally invasive hemorrhoid treatments, focusing on rubber band ligation (banding), sclerotherapy, and other outpatient options. You will learn how these procedures work, who they’re for, their benefits, risks, and what to expect.
Understanding Hemorrhoids and Their Treatment
Hemorrhoids come in two main types:
- Internal hemorrhoids: Occur inside the rectum, often painless but prone to bleeding and prolapse.
- External hemorrhoids: Develop under the skin around the anus, often painful and sometimes thrombosed.
Treatment depends on severity and symptoms, with hemorrhoids graded I to IV based on prolapse and symptom severity.
- Grade I & II: Typically treated with conservative care or minimally invasive procedures.
- Grade III & IV: May require more advanced interventions or surgery.
Minimally invasive procedures are ideal for Grades I to III hemorrhoids that don’t respond fully to home care.
1. Rubber Band Ligation (Banding)
What is Rubber Band Ligation?
Rubber band ligation (RBL) is the most commonly performed minimally invasive procedure for internal hemorrhoids. It involves placing a tiny rubber band around the base of the hemorrhoid to cut off its blood supply, causing it to shrink and eventually fall off.
How Is It Done?
- The procedure is performed in a doctor’s office without anesthesia.
- A special instrument called a ligator or anoscope is used to view the hemorrhoid.
- A rubber band is carefully placed around the base of the hemorrhoid.
- The band tightens, cutting off circulation.
- Within 5–7 days, the hemorrhoid shrinks and falls off during a bowel movement.
- The area heals with minimal scarring.
Who Is a Candidate?
- Best suited for Grade I to III internal hemorrhoids.
- Not typically used for external hemorrhoids.
- Patients with bleeding internal hemorrhoids who have not improved with conservative treatment.
Benefits
- Quick outpatient procedure.
- Minimal discomfort; no incisions.
- High success rate (about 70–90% effective).
- Low risk of complications.
Possible Side Effects
- Mild pain or discomfort for a few days.
- Minor bleeding after band falls off.
- Rarely, infection or significant pain requiring medical attention.
Aftercare
- Avoid heavy lifting and straining for a few days.
- Use stool softeners and a high-fiber diet to ease bowel movements.
- Follow up with your healthcare provider as advised.
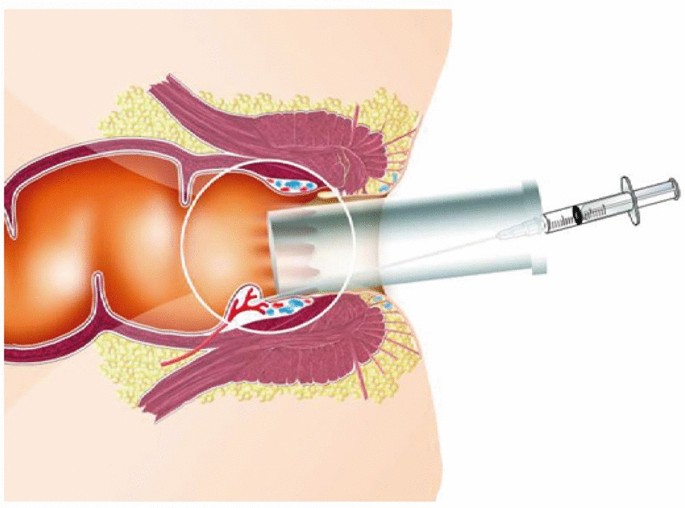
2. Sclerotherapy
What is Sclerotherapy?
Sclerotherapy is a procedure that involves injecting a chemical sclerosant directly into the hemorrhoid tissue. This causes inflammation and scarring, which shrinks the hemorrhoid and reduces symptoms.
How Is It Done?
- Typically performed in a doctor’s office.
- A small needle injects the sclerosant into the hemorrhoid.
- The solution irritates the blood vessels, causing them to shrink.
- Over several weeks, the hemorrhoid diminishes.
Who Is a Candidate?
- Suitable for small to moderate internal hemorrhoids (Grade I or II).
- Sometimes used for patients who cannot tolerate banding.
- Often used as an alternative or adjunct to banding.
Benefits
- Simple, quick outpatient procedure.
- Minimal pain and discomfort.
- Effective for bleeding hemorrhoids.
- Can be repeated if necessary.
Possible Side Effects
- Mild discomfort or burning sensation.
- Rare allergic reactions.
- Rarely, ulceration or bleeding.
Aftercare
- Avoid straining and heavy lifting.
- Maintain a high-fiber diet and hydration.
- Monitor for any unusual symptoms.
3. Infrared Coagulation (IRC)
What is IRC?
Infrared coagulation uses infrared light to generate heat, causing coagulation of hemorrhoidal tissue and blood vessels, leading to shrinkage.
How Is It Done?
- A probe applies infrared light pulses to hemorrhoid tissue.
- This causes the veins to harden and scar, reducing symptoms.
Who Is a Candidate?
- Ideal for small to medium internal hemorrhoids.
- Used when banding or sclerotherapy is contraindicated or as an adjunct.
Benefits
- Quick and painless.
- No anesthesia required.
- Minimal side effects.
Possible Side Effects
- Mild discomfort.
- Rare bleeding or ulceration.
4. Other Minimally Invasive Techniques
- Cryotherapy: Freezing hemorrhoid tissue to cause necrosis (less commonly used).
- Laser therapy: Using laser energy to shrink hemorrhoids.
- Doppler-guided hemorrhoidal artery ligation (DGHAL): Locates and ties off hemorrhoidal arteries to reduce blood flow and shrink hemorrhoids.
These are typically reserved for more specialized cases or larger hemorrhoids.
Comparing Minimally Invasive Procedures
| Procedure | Best for | Pain Level | Recovery Time | Effectiveness |
| Rubber Band Ligation | Grade I-III internal | Mild discomfort | Few days | High (70–90%) |
| Sclerotherapy | Grade I-II internal | Minimal | Immediate | Moderate to high |
| Infrared Coagulation | Small internal hemorrhoids | Minimal | Immediate | Moderate |
| DGHAL | Larger hemorrhoids | Moderate | Few days | Good |
Risks and Considerations
Though minimally invasive procedures are generally safe, risks include:
- Bleeding
- Infection
- Pain or discomfort
- Urinary retention (rare)
- Recurrence of hemorrhoids over time
It’s important to discuss your medical history and any medications with your healthcare provider before the procedure.
When Is Surgery Needed?
Minimally invasive treatments are effective for many, but severe hemorrhoids (Grade IV), large prolapsed hemorrhoids, or persistent symptoms may require surgical hemorrhoidectomy.
Conclusion
Minimally invasive hemorrhoid procedures such as rubber band ligation and sclerotherapy offer effective, low-risk, and convenient treatment options for many patients with internal hemorrhoids. These outpatient treatments provide symptom relief, quick recovery, and help avoid the discomfort and downtime associated with traditional surgery.
If you suffer from hemorrhoids that don’t respond to home care or cause significant discomfort, consult a healthcare professional to discuss if one of these minimally invasive procedures might be right for you.
FAQs:
What is rubber band ligation for hemorrhoids?
It’s a procedure where a small rubber band is placed around the base of an internal hemorrhoid to cut off blood flow, causing it to shrink and fall off.
Is sclerotherapy painful?
Sclerotherapy usually causes minimal discomfort; it involves injecting a chemical to shrink the hemorrhoid with little pain.
How long does recovery take after rubber band ligation?
Most people recover within a few days and can return to normal activities quickly.
Can these procedures treat external hemorrhoids?
Minimally invasive procedures like banding and sclerotherapy are mainly for internal hemorrhoids, not external ones.
Are there risks associated with these treatments?
Risks are low but can include mild pain, bleeding, infection, or hemorrhoid recurrence.