Introduction
Hemorrhoids—swollen and inflamed veins in the rectal and anal area—are a common health issue, affecting millions globally. While many mild to moderate cases respond well to lifestyle changes and minimally invasive treatments, severe hemorrhoids often require surgical intervention for lasting relief.
Hemorrhoidectomy, the surgical removal of hemorrhoids, remains the gold standard treatment for large, prolapsed, or thrombosed hemorrhoids that don’t improve with conservative care. This article explores what hemorrhoidectomy involves, who needs it, the types of surgery available, risks, recovery, and alternatives.
When Is Surgery Needed?
Surgery is generally considered when:
- Hemorrhoids are Grade III or IV, meaning they prolapse outside the anus and cannot be pushed back in.
- Patients suffer significant bleeding, pain, or thrombosis despite other treatments.
- Hemorrhoids are large and cause chronic symptoms or complications.
- Other treatments like rubber band ligation, sclerotherapy, or infrared coagulation fail.
- There are associated anal conditions (e.g., fistulas, fissures) requiring surgical management.
Understanding Hemorrhoidectomy
Hemorrhoidectomy is the surgical excision (removal) of hemorrhoidal tissue. It is usually performed under general, regional (spinal), or local anesthesia, depending on the extent of surgery and patient health.
Goals of Hemorrhoidectomy:
- Remove hemorrhoidal tissue causing symptoms
- Reduce bleeding, pain, and prolapse
- Restore normal anatomy and function of the anus
Types of Hemorrhoidectomy Procedures
1. Conventional (Open) Hemorrhoidectomy
- The most commonly performed surgical technique.
- The hemorrhoidal tissue is excised and left open to heal naturally.
- Performed under anesthesia, usually in an outpatient or short-stay hospital setting.
- Effective for large, prolapsed hemorrhoids.
Pros:
- High success rate.
- Complete removal of hemorrhoids.
Cons:
- Longer recovery time.
- More postoperative pain.
- Open wounds require careful hygiene and care.
2. Closed Hemorrhoidectomy
- Similar to the open method, but the wound is sutured closed after removal.
- May reduce healing time and pain compared to open surgery.
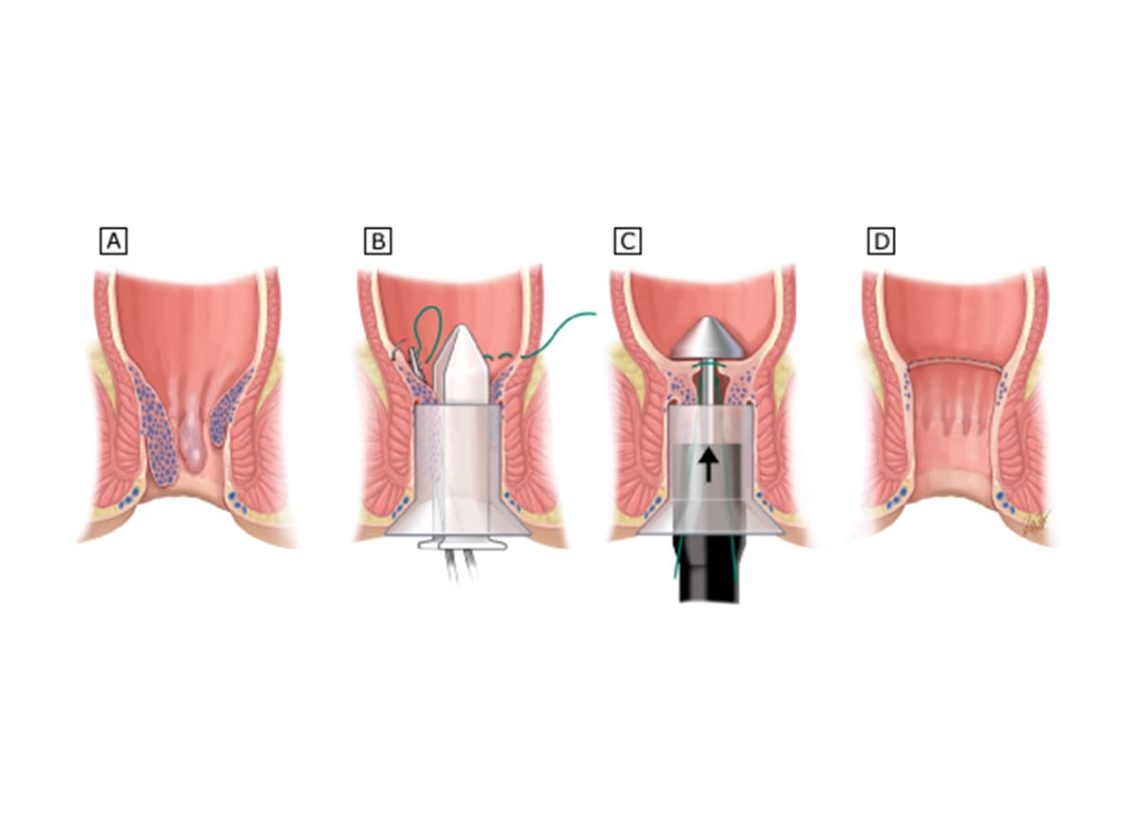
3. Stapled Hemorrhoidopexy (PPH – Procedure for Prolapse and Hemorrhoids)
- Uses a circular stapling device to reposition and staple prolapsed hemorrhoidal tissue back into place.
- Cuts off blood supply, causing the hemorrhoids to shrink.
- Less painful than traditional hemorrhoidectomy.
- Usually suitable for Grade III hemorrhoids.
Pros:
- Faster recovery.
- Less pain.
- Shorter hospital stay.
Cons:
- Higher recurrence risk compared to conventional surgery.
- Not ideal for thrombosed or very large hemorrhoids.
4. Hemorrhoidal Artery Ligation (HAL) or Doppler-Guided Hemorrhoidal Artery Ligation (DG-HAL)
- Uses Doppler ultrasound to locate and tie off hemorrhoidal arteries.
- Reduces blood flow, causing shrinkage of hemorrhoids.
- Less invasive, with shorter recovery.
Note: While not a full hemorrhoidectomy, HAL is a surgical option for severe cases.
What to Expect During Surgery
- Preoperative assessment including history, physical exam, and sometimes colonoscopy.
- Anesthesia administered.
- Surgery duration varies from 30 minutes to 1 hour.
- Often an outpatient or overnight hospital stay.
- Postoperative monitoring for pain and bleeding.
Postoperative Care and Recovery
Pain Management
- Pain after hemorrhoidectomy is common and can be significant.
- Managed with prescribed painkillers, sitz baths, and stool softeners.
Wound Care
- Keep the area clean with gentle washing after bowel movements.
- Sitz baths several times daily help reduce discomfort.
- Use of ointments or creams as prescribed.
Bowel Management
- Avoid constipation with a high-fiber diet and adequate fluids.
- Stool softeners or mild laxatives may be recommended.
Activity
- Rest for the first few days.
- Avoid heavy lifting and strenuous exercise for 2–4 weeks.
- Gradually resume normal activities as tolerated.
Risks and Complications
Though generally safe, hemorrhoidectomy has potential risks:
- Pain and discomfort (usually worst in the first week)
- Bleeding
- Infection
- Urinary retention (difficulty urinating)
- Narrowing of the anal canal (anal stenosis)
- Fecal incontinence (rare)
- Delayed wound healing
Close follow-up with your healthcare provider is important to manage any complications.
Alternatives to Surgery
For some patients, less invasive options may be preferable, including:
- Rubber band ligation
- Sclerotherapy
- Infrared coagulation
- Doppler-guided artery ligation
- Lifestyle changes and medical management
Your doctor can help determine the best approach based on your symptoms and overall health.
Conclusion
For patients suffering from severe, persistent hemorrhoids, hemorrhoidectomy offers a reliable and often definitive solution. Though recovery can be uncomfortable, surgery typically provides significant relief from bleeding, prolapse, and pain that other treatments fail to address.
Understanding the types of surgical options, what to expect before and after surgery, and potential risks will help you make informed decisions in consultation with your healthcare provider.
If your hemorrhoid symptoms significantly impact your quality of life and conservative treatments have not worked, discussing hemorrhoidectomy with a colorectal surgeon or specialist can be the next step toward lasting relief.
FAQs:
When is hemorrhoidectomy recommended?
It’s usually recommended for severe (Grade III or IV) hemorrhoids that don’t respond to other treatments or cause significant pain and prolapse.
What types of hemorrhoidectomy are there?
Common types include conventional open hemorrhoidectomy, closed hemorrhoidectomy, stapled hemorrhoidopexy, and artery ligation procedures.
How long is the recovery after a hemorrhoidectomy?
Recovery can take 2 to 4 weeks, with pain usually most intense in the first week after surgery.
What are the common risks of hemorrhoidectomy?
Risks include pain, bleeding, infection, urinary retention, and, rarely, anal stenosis or incontinence.
Are there less invasive alternatives to hemorrhoidectomy?
Yes, options like rubber band ligation, sclerotherapy, and infrared coagulation may be suitable for less severe cases.