Introduction
Hemorrhoids are common and often manageable at home with lifestyle changes and over-the-counter remedies. But in some cases, they can become persistent, painful, or signal a more serious issue. Knowing when to see a doctor for hemorrhoids is key to preventing complications, relieving discomfort, and ensuring that your symptoms aren’t caused by another condition like colorectal cancer or inflammatory bowel disease.
This article explains the warning signs that indicate it’s time to seek professional medical help, what to expect during a hemorrhoid evaluation, and treatment options your doctor might recommend.
Understanding Hemorrhoids
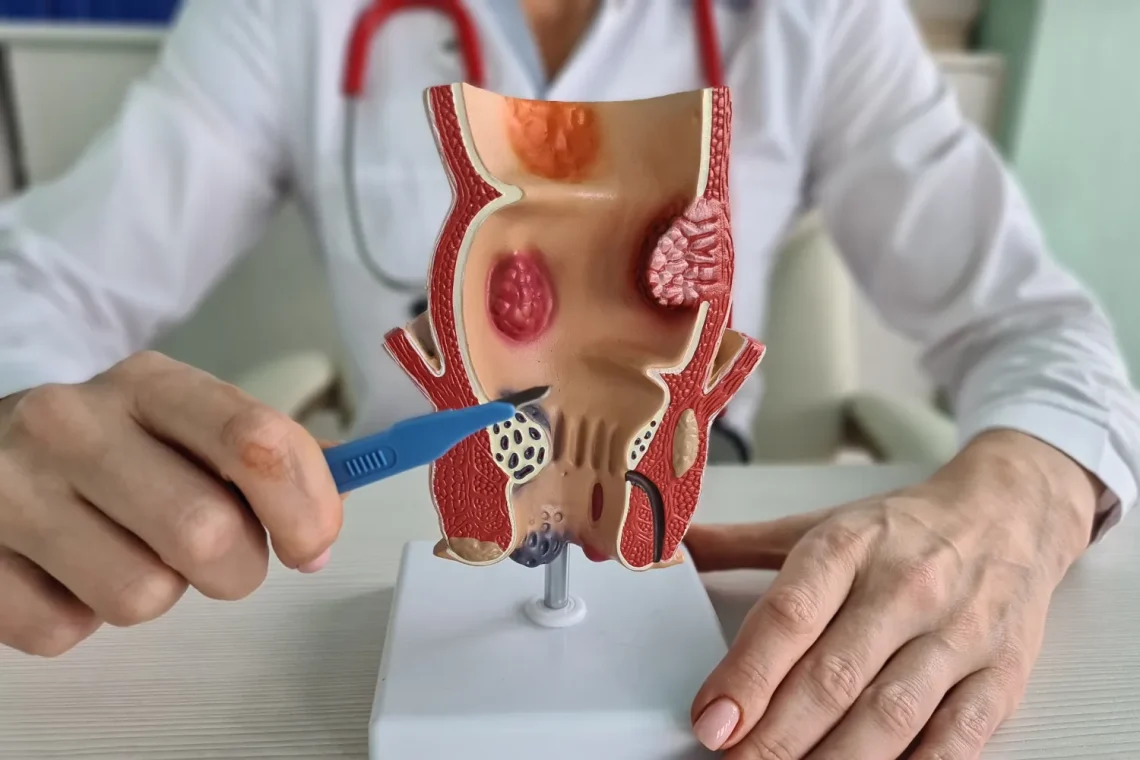
Hemorrhoids are swollen veins in the lower rectum or anus and are categorized as:
- Internal hemorrhoids – Located inside the rectum; often painless but may bleed.
- External hemorrhoids – Found under the skin around the anus; can be itchy, painful, or form clots (thrombosed).
Most people experience mild symptoms that improve with home care. But not all hemorrhoids are harmless, and some require medical evaluation and treatment.
Common Mild Symptoms That Often Respond to Home Care
Before jumping to medical care, it’s good to know which symptoms typically do not require urgent attention:
- Mild itching or irritation around the anus
- Bright red blood on toilet paper
- Occasional discomfort or fullness during bowel movements
- Small, soft lumps around the anus that shrink on their own
- Mild prolapse that resolves with gentle pressure
These can often be managed with sitz baths, high-fiber diets, hydration, and topical ointments.
When to See a Doctor for Hemorrhoids
You should schedule a medical appointment if you experience any of the following:
1. Persistent or Heavy Rectal Bleeding
- If you see bright red blood in the toilet, on the stool, or on toilet paper frequently.
- If the bleeding is heavy or occurs without bowel movements.
- If you feel lightheaded, dizzy, or fatigued (signs of anemia or blood loss).
Why it matters: Rectal bleeding could also be a sign of more serious conditions like colorectal cancer, anal fissures, diverticulosis, or inflammatory bowel disease (IBD). A doctor may recommend a colonoscopy or other screening tests.
2. Severe or Increasing Pain
- If you feel intense pain while sitting, walking, or having a bowel movement.
- If a painful lump develops rapidly, it could be a thrombosed external hemorrhoid.
- If over-the-counter pain relief doesn’t help.
Why it matters: Thrombosed hemorrhoids may require a minor surgical procedure (incision and drainage) for pain relief and to prevent complications.
3. Prolapsed Hemorrhoids That Don’t Go Back In
- Internal hemorrhoids may protrude outside the anus during bowel movements (prolapse).
- If they don’t retract on their own or cannot be gently pushed back in, medical care is needed.
Why it matters: Prolapsed hemorrhoids can become trapped, swollen, and painful, potentially leading to tissue damage or infection.
4. No Improvement After a Week of Home Treatment
- If you’ve tried sitz baths, dietary changes, and creams but symptoms persist or worsen after 7–10 days, see your doctor.
Why it matters: Chronic or severe hemorrhoids may need medical procedures like rubber band ligation, sclerotherapy, or surgery.
5. Recurring Hemorrhoids
- If you experience repeated episodes, especially despite lifestyle changes, professional guidance is needed.
Why it matters: Recurrent hemorrhoids may indicate a structural issue or chronic bowel habits that require medical evaluation and long-term strategies.
6. Changes in Bowel Habits or Stool Appearance
- If you notice thin, ribbon-like stools, mucus, or diarrhea alternating with constipation.
- If you have unexplained weight loss or persistent abdominal pain.
Why it matters: These can be signs of colorectal cancer or inflammatory bowel conditions—not just hemorrhoids.
What to Expect During a Doctor’s Visit
1. Medical History and Symptom Review
Your doctor will ask about:
- Frequency and type of bleeding
- Bowel habits
- Diet and fluid intake
- Family history of colon problems
2. Physical Examination
- Visual inspection (for external hemorrhoids)
- Digital rectal exam: To feel for internal hemorrhoids or other abnormalities
3. Diagnostic Tests (If Needed)
- Anoscopy or proctoscopy: To view internal hemorrhoids
- Colonoscopy or sigmoidoscopy: If you’re over 45 or have unexplained bleeding or risk factors for colon cancer
Treatment Options from a Doctor
Non-Surgical Treatments
- Rubber band ligation (for internal hemorrhoids): Cuts off blood supply, causing them to shrink
- Sclerotherapy: Injection of a solution to shrink the hemorrhoid
- Infrared coagulation: Light therapy that causes hemorrhoids to shrink
Surgical Options
- Hemorrhoidectomy: Surgical removal; best for large or severe hemorrhoids
- Stapled hemorrhoidopexy: Repositions prolapsed hemorrhoids and cuts off blood flow
Tips for Preventing Hemorrhoids From Returning
- Eat a high-fiber diet and drink plenty of water
- Avoid prolonged sitting on the toilet
- Respond promptly to bowel urges
- Exercise regularly
- Maintain a healthy weight
Conclusion
Most hemorrhoids are mild and manageable with at-home care, but certain symptoms are red flags that need medical attention. Persistent bleeding, severe pain, non-retracting prolapse, or changes in bowel habits shouldn’t be ignored. Seeing a doctor ensures a correct diagnosis and opens the door to more effective, lasting treatment options.
Don’t suffer in silence—if symptoms are disrupting your life, professional help is available and often highly effective.
FAQs:
When should I be concerned about hemorrhoid bleeding?
If bleeding is frequent, heavy, or occurs without a bowel movement, or if you’re feeling dizzy or fatigued, see a doctor promptly.
Is pain a sign that I need medical treatment for hemorrhoids?
Yes, severe or persistent pain, especially with a lump, may indicate a thrombosed hemorrhoid that requires medical attention.
What if my hemorrhoids won’t go back in?
If you have a prolapsed hemorrhoid that doesn’t retract or can’t be pushed in gently, you should consult a doctor—it may need a procedure.
How long should I try home treatments before seeing a doctor?
If your symptoms don’t improve within 7–10 days of home care, or they get worse, it’s time for a professional evaluation.
Could my hemorrhoid symptoms be something more serious?
Yes—rectal bleeding or changes in bowel habits may mimic hemorrhoids but signal more serious conditions like colon cancer or IBD. Always get checked if you’re unsure.