Introduction
Most people associate tick bites with Lyme disease. But ticks can carry and transmit multiple pathogens, sometimes at the same time, leading to what’s known as tick-borne co-infections. These infections can complicate diagnosis, delay treatment, and increase the severity of symptoms.
In this article, we’ll explore the most common tick-borne co-infections, how they’re transmitted, symptoms to watch for, testing, treatment options, and how to protect yourself.
What Are Tick-Borne Co-Infections?
A co-infection occurs when a tick transmits more than one disease-causing pathogen in a single bite. The most common tick species responsible for co-infections in the U.S. is the blacklegged tick (Ixodes scapularis), also known as the deer tick, which transmits:
- Borrelia burgdorferi (causes Lyme disease)
- Babesia microti (causes babesiosis)
- Anaplasma phagocytophilum (causes anaplasmosis)
- Borrelia miyamotoi (causes a relapsing fever-like illness)
- Powassan virus (a rare but serious viral infection)
Common Tick-Borne Co-Infections
1. Babesiosis
- Pathogen: Babesia microti (a protozoan parasite)
- Transmission: By blacklegged ticks; also through blood transfusion
- Symptoms:
- Fatigue
- Fever, chills
- Sweats
- Muscle aches
- Nausea
- Anemia and low platelets
- Special Risk: Can be severe or fatal in people over 50, immunocompromised individuals, or those without a spleen
- Treatment: Combination of atovaquone and azithromycin, or clindamycin and quinine in severe cases
2. Anaplasmosis
- Pathogen: Anaplasma phagocytophilum (a bacterium)
- Transmission: Blacklegged tick
- Symptoms:
- High fever
- Severe headaches
- Muscle pain
- Chills
- Nausea
- Confusion or neurologic symptoms (in severe cases)
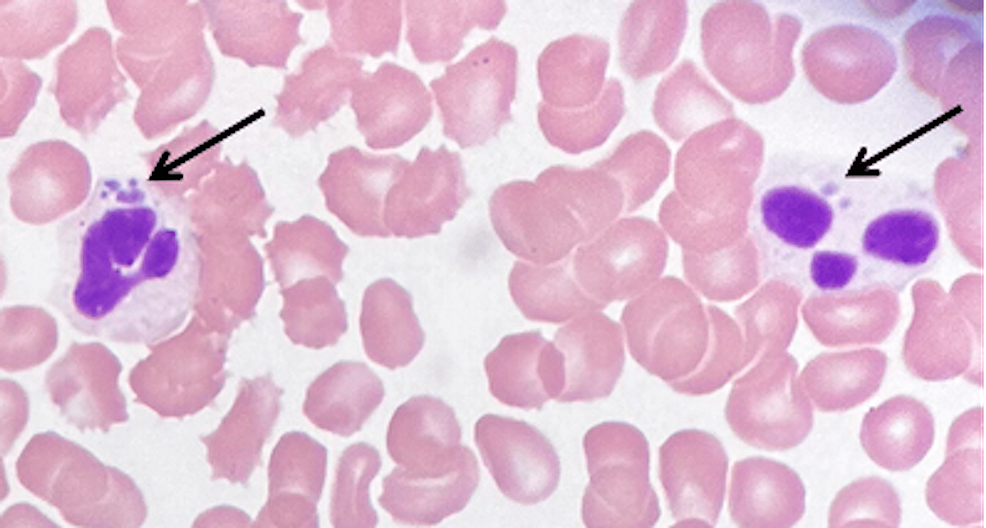
- Diagnosis: Blood smear, PCR, or antibody tests
- Treatment: Doxycycline (even in children and pregnant women in high-risk cases)
3. Ehrlichiosis
- Pathogen: Ehrlichia chaffeensis and others
- Transmission: Lone star tick (Amblyomma americanum)
- Symptoms:
- Fever
- Headache
- Malaise
- Rash (in some cases)
- Nausea, vomiting
- Treatment: Doxycycline (again, even in children under special guidance)
4. Powassan Virus
- Pathogen: Powassan virus (a flavivirus)
- Transmission: Blacklegged tick; virus can be transmitted in 15 minutes or less
- Symptoms:
- Fever
- Vomiting
- Weakness
- Seizures
- Encephalitis or meningitis (in severe cases)
- Treatment: No specific antiviral treatment; supportive care only
- Mortality: Around 10%; long-term neurologic damage possible in survivors
5. Borrelia Miyamotoi
- Pathogen: Borrelia miyamotoi (a spirochete similar to Lyme bacteria)
- Transmission: Blacklegged ticks
- Symptoms:
- Fever
- Chills
- Fatigue
- Headache
- Relapsing fever pattern
- Diagnosis: PCR or antibody tests (not usually detected on standard Lyme tests)
- Treatment: Doxycycline
Why Co-Infections Complicate Diagnosis and Treatment
- Overlapping symptoms make it hard to identify which pathogens are causing illness.
- Standard Lyme disease tests may miss co-infections.
- Some pathogens (like Babesia) are not killed by common Lyme antibiotics and need different drugs.
- Patients with co-infections often experience more severe symptoms, longer recovery times, and may be misdiagnosed as having chronic Lyme or other conditions.
Testing for Co-Infections
Ask for testing if:
- You live in or have traveled to tick-endemic areas
- You don’t respond to Lyme treatment as expected
- You experience symptoms like fever, chills, or anemia not typical of Lyme
Diagnostic Tools:
- PCR (for detecting pathogen DNA)
- Blood smear (especially for babesiosis)
- Antibody tests (serology)
- Complete blood count (may show anemia or low platelets)
Treatment Overview
| Infection | Main Treatment | Additional Notes |
| Lyme disease | Doxycycline or amoxicillin | 2–4 weeks typical |
| Babesiosis | Atovaquone + Azithromycin | Clindamycin + Quinine if severe |
| Anaplasmosis | Doxycycline | Begin treatment immediately if suspected |
| Ehrlichiosis | Doxycycline | Start treatment without delay |
| Borrelia miyamotoi | Doxycycline | Often confused with Lyme; needs PCR to confirm |
| Powassan virus | Supportive care only | No antiviral; hospitalization may be needed |
When to See a Doctor
Seek immediate medical attention if you have:
- Fever or chills within 1–4 weeks of a tick bite
- Unusual fatigue, night sweats, or headache
- Neurologic symptoms (confusion, seizures, slurred speech)
- Symptoms that worsen after Lyme treatment
Early detection and treatment of co-infections can greatly improve outcomes.
Prevention Tips
- Wear long sleeves and pants when in wooded or grassy areas
- Use EPA-approved tick repellents (DEET, permethrin-treated clothing)
- Shower and do a full-body tick check after being outdoors
- Check pets and gear
- Landscape your yard to reduce tick habitats
- Keep grass trimmed and remove leaf litter
Conclusion
Co-infections from ticks are a real and growing concern, particularly in regions where Lyme disease is common. Understanding that a tick bite may transmit more than one infection can lead to faster diagnosis, better treatment, and fewer complications.
If you’ve been bitten by a tick and experience symptoms that don’t fully match Lyme disease—or persist despite treatment—ask your doctor about possible co-infections like babesiosis, anaplasmosis, or ehrlichiosis. Early awareness is your best defense.
FAQs:
Can one tick bite cause more than one infection?
Yes, a single tick can transmit multiple pathogens at once, leading to co-infections like Lyme disease and babesiosis.
Are symptoms of co-infections different from Lyme disease?
Often, yes. Co-infections can cause fever, chills, sweats, or anemia, which aren’t typical of Lyme disease alone.
Do co-infections require different treatment?
Yes. Some co-infections, like babesiosis, require different medications than those used for Lyme disease.
How common are tick-borne co-infections?
In high-risk areas, 10–30% of people with Lyme disease may also have a co-infection.
How can I protect myself from tick-borne co-infections?
Use tick repellents, wear protective clothing, do full-body tick checks, and remove ticks quickly to lower your risk.