Introduction
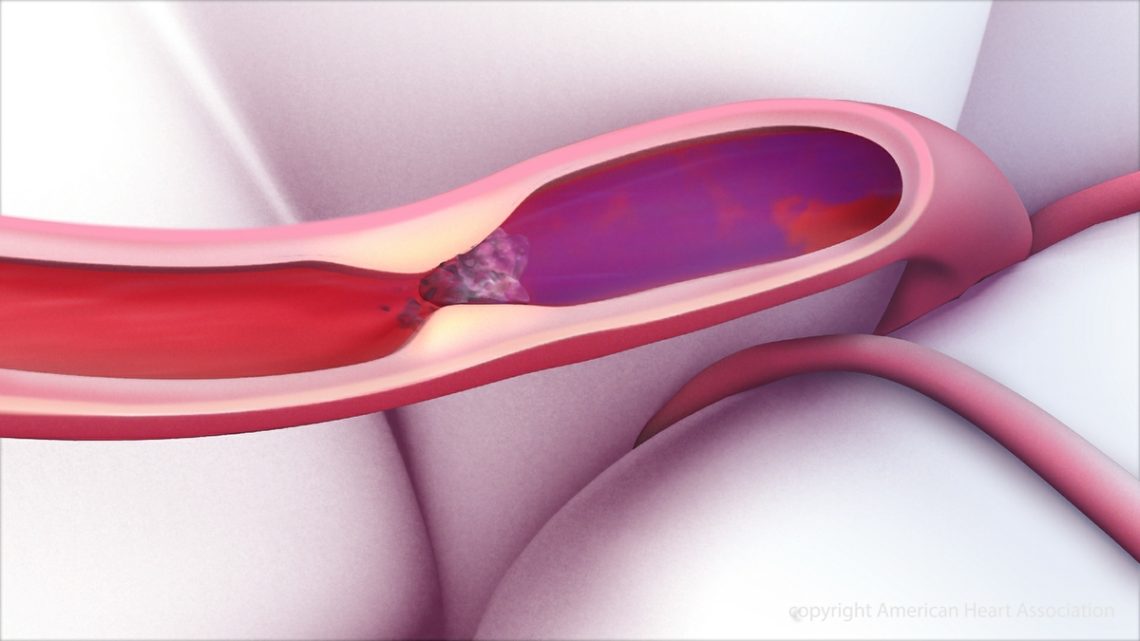
Stroke is a leading cause of disability and death worldwide. Prompt restoration of blood flow to the brain is critical in ischemic stroke, the most common type of stroke caused by a blood clot blocking a brain artery. Two highly effective treatments—clot-busting drugs (thrombolytics) and mechanical thrombectomy—have revolutionized stroke care by reopening blocked vessels and improving patient outcomes. This article explains how these treatments work, when they are used, and their importance in saving brain tissue.
Clot-Busting Drugs: Tissue Plasminogen Activator (tPA)
What is tPA?
tPA is a medication that dissolves blood clots by activating plasminogen, an enzyme that breaks down fibrin—the structural component of clots. It is the only FDA-approved intravenous thrombolytic for acute ischemic stroke.
How tPA Works
- Administered intravenously, tPA travels through the bloodstream to the clot site.
- It converts plasminogen into plasmin, which breaks down fibrin strands.
- This dissolves the clot, restoring blood flow to the affected brain area.
Eligibility and Timing
- tPA is most effective when given within 3 to 4.5 hours of stroke symptom onset.
- Patients must meet strict eligibility criteria to minimize risks, including:
- No recent surgery or bleeding
- No history of hemorrhagic stroke
- Blood pressure within safe limits
- No current anticoagulant use causing high bleeding risk
Benefits and Risks
- Significantly improves functional outcomes by limiting brain damage.
- Increases chances of regaining independence.
- Risk of bleeding (hemorrhagic transformation) is the major concern.
- Requires administration in hospitals with stroke expertise.
Mechanical Thrombectomy
What is Thrombectomy?
Mechanical thrombectomy is a minimally invasive procedure to physically remove a clot from a blocked brain artery. It is performed by neurointerventional specialists using advanced imaging guidance.
Procedure Overview
- A catheter is inserted through a large artery, usually in the groin.
- It is threaded up to the brain’s blocked artery.
- A stent retriever or suction device captures and removes the clot.
- Restores blood flow quickly, minimizing brain damage.
When is Thrombectomy Used?
- For large vessel occlusions in the brain, typically in the internal carotid artery or middle cerebral artery.
- Can be performed up to 24 hours after symptom onset in selected patients, based on imaging criteria.
- Often combined with intravenous tPA if the patient arrives early.
Benefits and Risks
- Dramatically improves outcomes in severe ischemic strokes.
- Expands treatment window beyond tPA alone.
- Risks include bleeding, vessel damage, and stroke recurrence.
Complementary Roles of tPA and Thrombectomy
- tPA is the first-line treatment if within the early time window and no contraindications.
- Thrombectomy is used for large clots not effectively treated by tPA or beyond tPA time window.
- Combining both treatments when appropriate maximizes chances of recovery.
Importance of Early Recognition and Treatment
- Time is brain: The faster blood flow is restored, the better the outcomes.
- Public awareness of stroke symptoms and rapid emergency response are critical.
- Hospitals with specialized stroke teams improve treatment access and success.
Conclusion
Clot-busting drugs like tPA and mechanical thrombectomy have transformed ischemic stroke treatment by rapidly reopening blocked vessels, saving brain tissue, and improving survivors’ quality of life. Early intervention, careful patient selection, and advanced techniques are key to maximizing their benefits and minimizing risks.
FAQs
How soon must tPA be given after stroke symptoms start?
Ideally, within 3 to 4.5 hours for maximum effectiveness.
Can everyone with ischemic stroke receive tPA?
No, eligibility depends on timing and medical conditions.
What is the success rate of thrombectomy?
Studies show significant improvement in functional outcomes, especially for large vessel strokes.
Are tPA and thrombectomy painful?
tPA is a medication infusion; thrombectomy is minimally invasive with sedation or anesthesia.
What happens if treatment is delayed?
Delayed treatment reduces effectiveness and increases brain damage.