Introduction
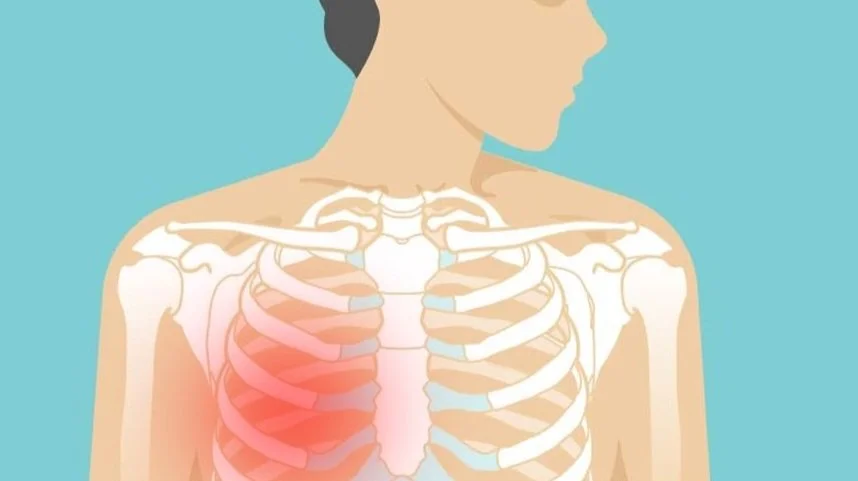
Chest pain is a symptom that often causes alarm, as many people immediately think of heart problems. However, not all chest pain is heart-related. One common cause of non-cardiac chest pain is costochondritis, an inflammation of the cartilage that connects the ribs to the breastbone (sternum). While it can be uncomfortable and even mimic heart attack pain, costochondritis is usually harmless and treatable.
What is Costochondritis?
- Costochondritis is the inflammation of the costal cartilage at the front of the rib cage.
- It most commonly affects the upper ribs, especially where they meet the sternum.
- Pain may feel sharp, aching, or pressure-like and can be reproduced by pressing on the affected area.
Causes and Risk Factors
The exact cause is not always clear, but common triggers include:
- Physical strain: heavy lifting, vigorous exercise, or repeated movement.
- Chest trauma: injury or impact to the chest.
- Respiratory infections: coughing can strain the chest wall.
- Arthritis: conditions like rheumatoid arthritis or ankylosing spondylitis.
- Unknown causes: sometimes costochondritis develops without a clear trigger.
Symptoms of Costochondritis
- Localized pain and tenderness along the sternum and rib joints.
- Pain worsens with:
- Deep breathing
- Coughing or sneezing
- Physical activity or movement of the upper body
- Pressure on the chest wall
- Unlike heart pain, costochondritis does not cause symptoms like sweating, nausea, or radiation to the arm/jaw (though overlap can sometimes confuse diagnosis).
Diagnosing Costochondritis
Because chest pain can be heart-related, doctors first rule out cardiac causes with:
- EKG (Electrocardiogram)
- Blood tests (Troponin)
- Chest X-ray
Once heart disease and lung problems are excluded, the diagnosis is made by:
- Physical exam: pain is reproducible when pressing on the affected cartilage.
- Medical history: recent strain, infection, or injury.
Treatment and Management
1. Medications
- NSAIDs (e.g., ibuprofen, naproxen) to reduce pain and inflammation.
- Topical pain relievers (creams, gels, patches).
2. Lifestyle Measures
- Rest and avoid activities that worsen pain.
- Apply heat or ice packs to the chest area.
- Practice gentle stretching to ease stiffness.
3. Physical Therapy
- Helps improve posture, flexibility, and reduce recurrence.
4. Injections (for severe cases)
- Corticosteroid injections into the inflamed area may be used if pain persists.
Prognosis
- Costochondritis is generally benign and self-limiting.
- Most people recover within a few weeks to a few months.
- Some may experience recurrent flare-ups, especially with physical strain.
When to See a Doctor
Seek urgent medical attention if chest pain is accompanied by:
- Shortness of breath
- Sweating, dizziness, or nausea
- Pain radiating to the arm, neck, or jaw
- History of heart disease or risk factors
⚠️ Rule of thumb: Always err on the side of caution with chest pain until cardiac causes are excluded.
Conclusion
Costochondritis is a common but often misunderstood cause of chest pain. While it can be alarming, it is not heart-related and usually resolves with rest, anti-inflammatory treatment, and lifestyle adjustments. Recognizing its signs and distinguishing it from more serious causes of chest pain helps patients avoid unnecessary worry while still seeking timely medical care when needed.
FAQs
1. Can costochondritis feel like a heart attack?
Yes. The pain can be sharp and located near the breastbone, which is why doctors must rule out cardiac causes first.
2. How long does costochondritis last?
It often resolves within weeks to months, but flare-ups may occur.
3. Can exercise make costochondritis worse?
Yes. High-intensity or chest-focused exercises can aggravate inflammation. Gentle movement is recommended.
4. Is costochondritis dangerous?
No, it is not life-threatening. The main concern is distinguishing it from heart-related chest pain.
5. Can stress cause costochondritis?
Stress does not directly cause it, but tension and muscle strain may worsen symptoms.