Introduction
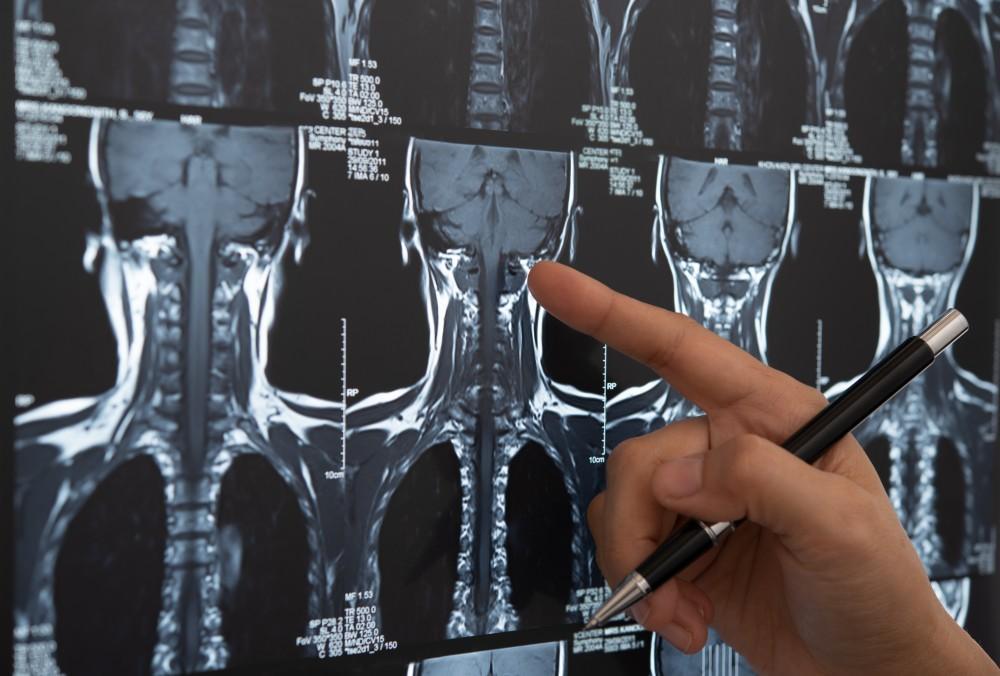
Back pain is one of the most common health complaints worldwide. While most cases of acute low back pain are self-limiting and improve within a few weeks, imaging tests such as X-rays, MRI, or CT scans are sometimes necessary to identify serious underlying conditions. However, routine imaging for all back pain is not recommended, as it may not improve outcomes and can lead to unnecessary interventions.
Understanding when imaging is appropriate, which type of test to choose, and what information it provides is crucial for both patients and clinicians.
Why Imaging Isn’t Always Needed
Most acute back pain is caused by:
- Muscle strain
- Ligament sprain
- Mild disc irritation
These conditions usually heal with rest, exercise, and conservative care. Imaging is often unnecessary unless red flags or persistent symptoms are present. Overuse of imaging can:
- Increase healthcare costs
- Lead to unnecessary treatments
- Causes anxiety due to incidental findings
Red Flags Indicating the Need for Imaging
Imaging is warranted when serious underlying conditions are suspected. Red flags include:
1. Neurological Deficits
- Leg weakness or foot drop
- Loss of sensation in the legs
- Loss of reflexes
2. Bladder or Bowel Dysfunction
- Difficulty controlling urination or bowel movements
- Could indicate cauda equina syndrome, a medical emergency
3. Severe or Progressive Pain
- Pain that worsens despite rest and medications
- Night pain preventing sleep
4. Trauma
- Recent fall, car accident, or injury
- Suspected fracture or spinal instability
5. History of Cancer
- Previous cancer with new back pain could indicate spinal metastasis
6. Infection or Fever
- Fever, chills, or unexplained weight loss may suggest spinal infection
7. Chronic or Recurrent Pain
- Pain persisting more than 6–12 weeks
- Repeated episodes affecting quality of life
Types of Imaging Tests for Back Pain
1. X-ray
- Purpose: Detects bone fractures, spinal alignment issues, arthritis, and degenerative changes.
- Limitations: Cannot show soft tissues like discs, nerves, or muscles.
- Best For: Trauma, suspected fractures, chronic arthritis evaluation.
2. MRI (Magnetic Resonance Imaging)
- Purpose: Detailed view of soft tissues—discs, spinal cord, nerves, ligaments, and muscles.
- Advantages: Non-invasive, no radiation exposure
- Best For: Suspected herniated discs, nerve compression, spinal infections, or tumors
3. CT Scan
- Purpose: More detailed bone imaging than X-ray
- Best For: Complex fractures or surgical planning
4. Bone Scan
- Purpose: Detects infections, fractures, or tumors in bones
- Used When: Standard imaging is inconclusive
Guidelines for Imaging
Acute Low Back Pain (<6 weeks)
- No red flags: Imaging is usually not recommended
- Red flags present: Immediate imaging (X-ray or MRI) is warranted
Chronic Low Back Pain (>6–12 weeks)
- Persistent pain or neurological symptoms may require MRI to identify disc, nerve, or spinal cord problems
Post-Trauma
- X-ray or CT to rule out fractures or instability
Suspected Serious Conditions
- MRI for infection, tumor, or severe nerve compression
Risks and Considerations
- Radiation exposure: Mainly from X-rays and CT scans
- Incidental findings: Abnormalities unrelated to symptoms may lead to unnecessary interventions
- Cost: MRI and CT scans are expensive
- Claustrophobia or metal implants: May limit MRI use
Non-Imaging Evaluation First
Before imaging, doctors often rely on:
- Thorough medical history
- Physical examination
- Assessment of pain pattern, reflexes, and muscle strength
- Trial of conservative treatment (rest, physical therapy, medications)
Imaging is reserved for cases where diagnosis is uncertain or serious conditions are suspected.
Conclusion
Most back pain resolves without imaging. Tests like X-rays, MRI, and CT scans are reserved for specific cases with red flags, persistent symptoms, trauma, or suspected serious conditions. Understanding when imaging is needed prevents unnecessary procedures, reduces healthcare costs, and ensures that serious problems are diagnosed promptly. A careful clinical evaluation combined with targeted imaging provides the best approach to managing back pain effectively.
FAQs
1. Should everyone with back pain get an MRI?
No, MRI is only recommended if red flags are present or pain persists beyond 6–12 weeks.
2. Can X-rays detect herniated discs?
No, X-rays show bones but cannot visualize discs or nerves; MRI is preferred for soft tissues.
3. Is it safe to get repeated X-rays or CT scans?
Repeated imaging increases radiation exposure, so tests are only done when necessary.
4. How long should I try conservative care before imaging?
Typically, 6 weeks of conservative treatment is recommended if no red flags exist.
5. Can imaging findings guide treatment?
Yes, MRI and CT can help doctors plan surgery or targeted therapy, but mild findings without symptoms may not require treatment.